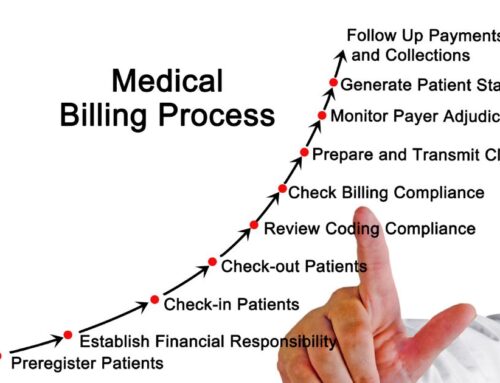
To effectively track healthcare revenue cycle performance, provider organizations should adopt several key performance indicators or KPIs. These metrics provide hospital and practice leaders with a strategic goal focused view of how the organization is operating. Credence Global Solutions has developed a list of the top 5 healthcare KPIs that providers and practitioners can implement to effectively track their revenue and resource cycle management.
Revenue Cycle Management
The advantage of determining your revenue cycle efficiency is it sets the standard for all other KPIs to be measured against. You can see very quickly if your practice is aimed towards the right direction. When it isn’t you can use this KPI to determine the appropriate strategy to turn things around in a 30, 60, or 90 day cycle. Managing resource availability and your workforce are imperative for this metric. With Credence resource management tools and expertise, tailored strategies can be engineered and fit to your organization on your timeline.
1. Calculating Net Days in Accounts Receivable
The net days in A/R shows a provider organization a very tangible measure of revenue cycle efficiency. This can be achieved by dividing the net A/R by the average daily net patient service revenue. The information needed to calculate this stems from an organization’s balance sheet and income statement. For clarification, net A/R is the net patient receivables on the balance sheet and it comprises the net of credit balance, allowances for uncollectible accounts, charity care discounts, and contractual allowance for third party payers. The total list of data needed includes:
– A/R receivables outsourced to third-party entities, but not considered bad debt
– Payments from the Medicare Disproportionate Share Hospital (DSH) program
– Medicare Indirect Medical Education (IME) paid on a Medicare Severity-Diagnosis Related Group (MS-DRG) account by account basis
– A/R associated with a patient-specific third-party settlement
– Critical access hospital payments and settlements
Provider organizations should not include non-patient A/R, 340B Drug Purchasing Program revenue, capitation or premium revenue from value-based contracts, and A/R related to non-patient-specific third-party settlements (eg, payments from Medicaid DSH and Direct Graduate Medical Education programs).
The KPI also excludes payments for any state or county subsidy, ambulance services, tax, and match type assessments, retail pharmacy, post-acute services, and physician practice/clinic unless the clinic is a Medicare recognized provider-based status clinic.
2. Cash Collection as a Percentage of Net Patient Services Revenue
The purpose of this metric is to evaluate an organization’s financial health by understanding its revenue cycle’s ability to transfer net patient services revenue into cash. This KPI can be calculated by dividing the collected patient service cash, found on the balance sheet, by the average monthly net patient service revenue, which is on the income statement.
Provider organizations should exclude some total collected patient service cash from this calculation. This includes patient-related settlements and payments, such as a safety net. Leaders should also avoid non-patient cash as well as collected patient service cash from ambulance services, post-acute services, and physician practices and clinics unless they are recognized as a provider-based clinic by Medicare
3. Claim Denial Rate
This indicator tracks the percentage of claims denied and shows an organization its payer compliance capabilities as well as the ability of its payers to accurately reimburse claims. Organizations can calculate this by dividing the total number of claims denied by the aggregate number of claims remitted. This information is found in A/R.
4. Final Denial Write-Off as a Percentage of Net Patient Services Revenue
This indicator permits provider organizations to monitor lost claims reimbursement after all appeal efforts when providers elect to write-off expected revenue. Hospital and practice leaders can find the KPI by dividing the net dollars written off as claim denials as found on the patient financial system by the average monthly net patient service revenue.
5. Cost to Collect
Leaders can find the rate by dividing the total revenue cycle cost as found on the income statement by the total patient service cash collected, which is on the balance sheet. Revenue cycle costs do not represent hard health IT costs, such as hardware expenses, licensing fees, server expenses, and any full-time equivalent staff that support the systems. The costs also exclude lease and rent costs, physical space expenses, and scheduling if the function is performed in the service departments by their staff.
Whether an organization defines peer groups by state, Medicare contractor region, bed number, or net patient service revenue, understanding how its revenue cycle performs compared to the cycles of its peers will allow leaders to set goals for improvement and remain a market competitor. Developing these KPI’s Credence Global Solutions, and their team for Credence Medical Billing can guarantee better analysis of your organization’s goals and how effectively you meet them.